Headache specialists offer tips for surviving, avoiding neurological discomfort
It’s not just a headache. It isolates and incapacitates.
Those who suffer from migraines say they often feel as if the only people who understand the level of pain and life disruption they endure are fellow migraine sufferers.
A Nielson survey funded by Eli Lilly and Company found they are correct: Non-migraine sufferers who were surveyed underestimated the severity of pain caused by migraine headaches and underestimated the duration of a typical migraine.
According to the National Headache Foundation, nearly 40 million people in the U.S. have migraine or headache neurological disorders. Whether you experience migraines or know someone who does, September, which is Pain Awareness Month, is a good time to learn more about the differences between migraines and other types of headaches.
Headache specialists from the University of Mississippi Medical Center have a few tips for surviving – or maybe even avoiding – the next big one.
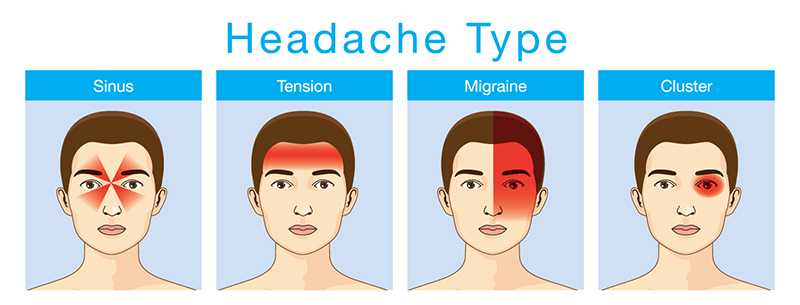
The World Health Organization divides headache disorders into three primary categories: migraine, tension and cluster headaches.

“Migraines usually start out on one side of the head,” said Liz Williams, family and psychiatric nurse practitioner in the Department of Neurology at UMMC who treats headache patients at both University Physicians Grants Ferry and the Jackson Medical Mall Thad Cochran Center. “Patients usually describe tension headaches as a band squeezing across the top of their forehead.”
Williams said common migraine symptoms also include:
- Nausea and sometimes vomiting,
- Visual changes, such as blurry vision, flashes of light or seeing spots before or during the headache,
- Sensitivity to light and sound,
- Inability to go about one’s regular activities and
- Changes in taste and smell.
"The migraine tends to be a pulsating, throbbing headache,” said Dr. Anand Prem, assistant professor of anesthesiology at UMMC. He sees patients at the Jackson Medical Mall Thad Cochran Center as a part of UMMC’s Pain Management Center.
Some people may experience an ‘aura’ before onset of the headache where they may see flashes of light or squiggly lines, while others can have hearing or smell abnormalities,” Prem said. “Some people can temporarily lose sensation or have tingling or numbness, especially around the jaw and face.”
Williams and Prem said most of their patients want to retreat to a dark quiet room until the headache subsides. They also agree that one of the best ways to deal with migraines is to learn your personal triggers.
Common triggers can include:
- Lack of or too much sleep,
- Skipping meals,
- Certain foods (especially those containing MSG and tyramine),
- Too much caffeine or not enough caffeine,
- Stress
- Change in hormones (women are more likely to experience migraines at the beginning of their menstrual cycle when estrogen levels drop),
- Weather changes (drops in barometric pressure) and
- Alcohol consumption.
“It helps to identify the triggers that may be a product of the environment so that you can try to avoid them,” Prem said.
Williams suggests a couple of phone apps to help patients identify their personal triggers: Migraine Buddy for Android and iHeadache for iPhone users.
“Everyone uses their phone now instead of journaling,” she said. “The apps are an easy way for patients to input their migraine information once they are feeling better.
“When they come back to the clinic, the patient will pull up the information in the app, and I can see how many migraines they had the previous month or week and the severity of the headaches.”
Williams and Prem emphasize the importance of knowing the warning signs and starting treatment early. They said not to wait until the headache is a full-blown migraine with all the worst symptoms.“If you feel that you are getting a migraine, be proactive and start the treatment early,” Williams said. “If you wait, sometimes the headache can get really bad and last longer.”

Prem warns that taking too much medication can cause what is commonly known as a rebound headache.
“You can begin to take the medication because you have a headache and then have a headache because you took the medication,” he said. “You are chasing your tail.”
He suggests if a patient is taking pain medication more than two times a week, he or she would benefit from taking a preventative medication rather than treating the pain after it starts.
Although much research is still being done to understand how to treat migraines, there are some common methods to help chronic migraine sufferers get relief. Newer treatments include addressing chemical changes in the brain and blocking nerves near where the pain occurs.
Because every patient is different, pinpointing the best course of treatment may take time and effort.
“Because there is no lab test to identify migraines, a health care provider has to really learn the patient,” Williams said. “I think the important thing is getting to know the patient.”
UMMC offers multiple clinics and health care providers to help people suffering from frequent headaches. Physician referrals are not necessary. Call 1-888-815-2005 and ask for an appointment with the Neurology Clinic or the Pain Management Center.


